At what age are men typically advised to begin discussing prostate cancer screening with their doctor?

Understanding Prostate Cancer Screening Guidelines
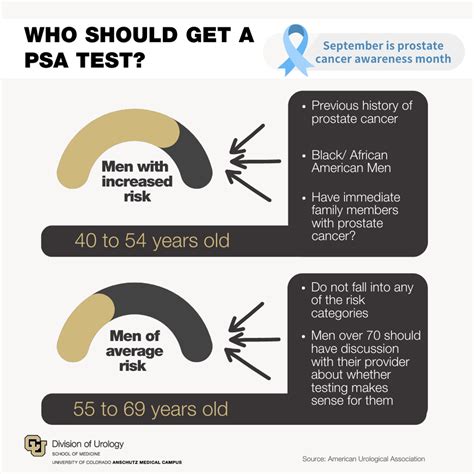
The question of when men should begin discussing prostate cancer screening with their doctor is a critical one, yet it doesn’t have a single, universal answer. Instead, it’s a nuanced conversation that takes into account individual risk factors, family history, ethnic background, and personal values. Major health organizations provide guidelines, but they all emphasize shared decision-making between a patient and their healthcare provider.

General Recommendations for Average-Risk Men
For men at average risk of prostate cancer, most medical organizations, including the American Cancer Society (ACS) and the American Urological Association (AUA), suggest that discussions about screening should begin around age 50. This age is considered a benchmark for initiating an informed conversation about the potential benefits and harms of screening.
An “average risk” man is generally defined as someone with no close relatives (father, brother, son) who had prostate cancer before age 65, and no other significant risk factors.
Earlier Discussions for High-Risk Groups
Certain groups of men face a higher risk of developing prostate cancer and are typically advised to start these discussions at an earlier age:
- African American Men: Due to a higher incidence and mortality rate from prostate cancer, African American men are often encouraged to begin discussions as early as age 40 or 45.
- Men with a Family History: If a man has a father, brother, or son who had prostate cancer before age 65, his risk increases. For these individuals, discussions should ideally start around age 40 or 45. The risk is even higher if multiple close relatives were affected at an early age.

Understanding the Screening Process: PSA and DRE
Prostate cancer screening typically involves two main tests:
- Prostate-Specific Antigen (PSA) Blood Test: This measures the level of PSA, a protein produced by prostate cells. Elevated PSA levels can indicate prostate cancer, but can also be caused by other conditions like benign prostatic hyperplasia (BPH) or infection.
- Digital Rectal Exam (DRE): During a DRE, a doctor manually checks the prostate for abnormalities like lumps or hard areas.
It’s crucial to understand that an elevated PSA or an abnormal DRE does not necessarily mean cancer; further diagnostic tests, such as a biopsy, are often required to confirm a diagnosis.
Weighing the Pros and Cons of Screening
The decision to screen is complex because while screening can detect prostate cancer early, potentially leading to curative treatment, it also carries potential harms:
- Potential Benefits: Early detection can lead to successful treatment, especially for aggressive cancers, and may reduce the risk of death from prostate cancer.
- Potential Harms:
- False Positives: High PSA levels can occur without cancer, leading to anxiety and unnecessary biopsies.
- Overdiagnosis and Overtreatment: Screening can find slow-growing cancers that may never cause symptoms or problems during a man’s lifetime. Treating these cancers can lead to side effects like erectile dysfunction, urinary incontinence, and bowel problems, without improving life expectancy.

The Importance of Shared Decision-Making
Given the complexities, medical experts strongly advocate for “shared decision-making.” This means that you and your doctor discuss your personal risk factors, your life expectancy, your preferences, and your values. Your doctor should explain the potential benefits, risks, and uncertainties of screening so you can make an informed choice that aligns with your health goals.
This discussion isn’t just about whether to get screened, but also about the frequency of screening and what follow-up actions would be taken based on the results.
Conclusion
There’s no single “right” age for every man to begin discussing prostate cancer screening. For most men, it’s typically around age 50, but for those with higher risk factors—such as African American men or those with a strong family history—these crucial conversations should start earlier, often between ages 40 and 45. Ultimately, the decision to screen is a deeply personal one, best made in collaboration with your healthcare provider after a thorough discussion of all relevant factors.