What are the current recommendations for prostate cancer screening in men without symptoms?
Prostate cancer is one of the most common cancers among men, yet screening for it in those without symptoms remains a complex and often debated topic. Unlike some other cancer screenings, a universal consensus on when and how to screen men for prostate cancer without any presenting symptoms is elusive, leading to varying recommendations from different medical organizations.
Understanding the Nuance of Prostate Cancer Screening
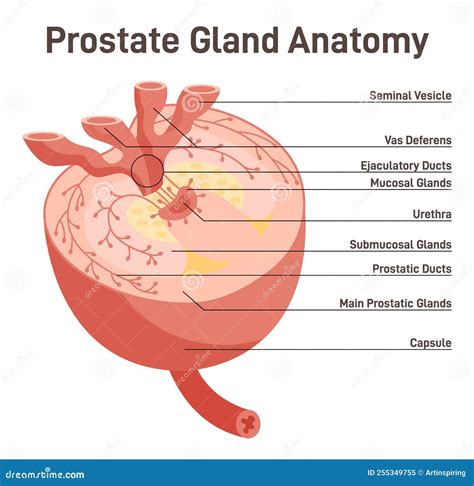
The primary goal of cancer screening is to detect cancer early, ideally before it causes symptoms, when treatment might be more effective. For prostate cancer, screening typically involves a Prostate-Specific Antigen (PSA) blood test and sometimes a digital rectal exam (DRE). However, the PSA test is not perfect; it can elevate due to non-cancerous conditions and may lead to overdiagnosis and overtreatment of slow-growing cancers that would never have caused harm.

Key Organizations and Their Guidelines
U.S. Preventive Services Task Force (USPSTF)
The USPSTF, a highly influential panel, provides graded recommendations based on evidence of benefits and harms. For men aged 55 to 69, the USPSTF recommends individual decision-making. This means that men in this age group should discuss the potential benefits and harms of screening with their doctor. Factors to consider include family history, ethnic background, and personal values. For men aged 70 and older, the USPSTF recommends against PSA-based screening, citing that the potential harms outweigh the benefits in this age group.
American Cancer Society (ACS)
The ACS also advocates for shared decision-making, starting at specific ages based on risk factors:
- Age 50 for men at average risk of prostate cancer and a life expectancy of at least 10 years.
- Age 45 for men at high risk, including African American men and those with a first-degree relative (father, brother, or son) diagnosed with prostate cancer before age 65.
- Age 40 or 45 for men at even higher risk, such as those with several first-degree relatives who had prostate cancer at an early age.
The ACS emphasizes that if a man decides to be tested, it should be after an informed discussion with their healthcare provider about the uncertainties, risks, and potential benefits of screening.

American Urological Association (AUA)
The AUA generally aligns with the shared decision-making approach. They recommend:
- For men aged 55 to 69 years, shared decision-making is recommended, with a strong emphasis on informed consent.
- For men aged 40 to 54 years, routine screening is not recommended in men at average risk. However, it may be offered to men at higher risk (e.g., strong family history, African American men) after discussion.
- For men over 70 years or any man with a life expectancy of less than 10-15 years, routine screening is not recommended.
The Concept of Shared Decision-Making
Shared decision-making is central to current prostate cancer screening recommendations. It involves a conversation between a man and his doctor to weigh the potential benefits and harms of screening in the context of his individual health status, values, and preferences.
Potential Benefits
- Early detection of potentially aggressive prostate cancer.
- Reduced risk of metastatic disease and death from prostate cancer in some men.
Potential Harms
- False positives: A high PSA level that is not due to cancer, leading to anxiety and unnecessary follow-up procedures like biopsies.
- Overdiagnosis: Detection of slow-growing, non-aggressive cancers that would never have caused symptoms or threatened a man’s life.
- Overtreatment: Treatment for these non-threatening cancers can lead to side effects such as erectile dysfunction, urinary incontinence, and bowel problems, significantly impacting quality of life.
Conclusion
For men without symptoms, there are no universal, one-size-fits-all recommendations for prostate cancer screening. Instead, the current guidelines from major health organizations emphasize a personalized approach rooted in shared decision-making. It is crucial for men, especially those aged 55-69, to have an open and thorough discussion with their healthcare provider to understand their individual risk factors, the potential benefits and harms of screening, and to make an informed choice that aligns with their personal values and health goals. Regularly reviewing this decision as health status changes or new evidence emerges is also advisable.