What are some lesser-known risk factors for cardiovascular disease that disproportionately affect men?

Beyond the Usual Suspects: Understanding Unique Male CVD Risks
While classic cardiovascular disease (CVD) risk factors like high cholesterol, hypertension, diabetes, and obesity are well-documented for both sexes, certain less-publicized factors disproportionately affect men, often going unnoticed until advanced stages. Understanding these unique risk factors is crucial for early detection, prevention, and tailored interventions to improve men’s long-term heart health.
This article delves into some of these overlooked contributors, from specific physiological conditions to lifestyle and treatment-related challenges, shedding light on how they uniquely impact the male cardiovascular system.

Erectile Dysfunction (ED): A Warning Sign for the Heart
Erectile dysfunction is often perceived as merely a sexual health issue, but it can be a significant early warning sign for underlying cardiovascular disease. ED occurs when blood vessels supplying the penis become narrowed or damaged, a process known as atherosclerosis, which is the same pathology that leads to heart attacks and strokes. Because the penile arteries are much smaller than coronary arteries, they often show signs of damage first.
Research indicates that men with ED, especially those under 50, are at a significantly higher risk of experiencing a cardiovascular event within the next few years, even if they have no other traditional risk factors. Therefore, ED should prompt a comprehensive cardiovascular evaluation, not just a prescription for ED medication.
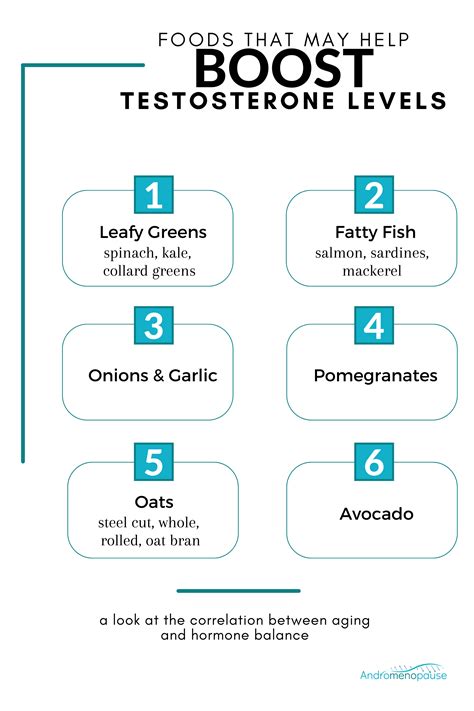
The Hidden Impact of Low Testosterone (Hypogonadism)
Low testosterone, or hypogonadism, is a condition that primarily affects men and is increasingly recognized for its potential links to cardiovascular health. While the relationship is complex and still being researched, studies suggest that men with chronically low testosterone levels may have an increased risk of coronary artery disease, metabolic syndrome, and type 2 diabetes—all significant contributors to CVD.
Symptoms of low testosterone, such as fatigue, reduced libido, depression, and loss of muscle mass, can overlap with other conditions, making diagnosis tricky. If diagnosed, a holistic approach to treatment that considers cardiovascular implications is essential.

Sleep Apnea: A Silent Threat
Obstructive sleep apnea (OSA) is a common but often undiagnosed sleep disorder characterized by repeated pauses in breathing during sleep. While it affects both genders, men, particularly middle-aged and overweight men, are disproportionately affected. OSA is a major, yet often overlooked, risk factor for high blood pressure, heart attack, stroke, and irregular heart rhythms (arrhythmias).
The repeated oxygen deprivation and stress on the cardiovascular system caused by OSA can lead to profound long-term damage. Symptoms like loud snoring, daytime fatigue, and morning headaches should prompt medical evaluation, as effective treatments like CPAP therapy can significantly reduce cardiovascular risk.

Chronic Stress, Mental Health, and Social Factors
Societal expectations often encourage men to internalize stress, avoid discussing emotional challenges, and delay seeking help for mental health issues like depression and anxiety. This stoicism can have serious cardiovascular consequences. Chronic stress elevates cortisol levels, blood pressure, and inflammation, all of which are detrimental to heart health.
Furthermore, untreated depression and anxiety are independently linked to an increased risk of heart disease and poorer outcomes after a cardiovascular event. Recognizing and addressing mental health concerns through therapy, stress management techniques, and open communication is a vital, yet often neglected, component of men’s heart health.

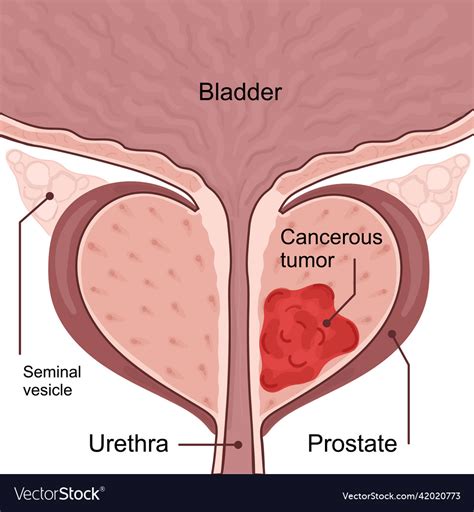
Androgen Deprivation Therapy (ADT) and Prostate Cancer
For men undergoing treatment for prostate cancer, particularly those receiving androgen deprivation therapy (ADT), there’s an increased risk of cardiovascular complications. ADT works by reducing testosterone levels, which can lead to adverse metabolic changes, including increased body fat, insulin resistance, and elevated cholesterol and triglyceride levels. These changes collectively raise the risk of developing metabolic syndrome and subsequent CVD.
It’s crucial for men undergoing ADT to have their cardiovascular health closely monitored by their oncology and cardiology teams, with proactive management of emerging risk factors.
Conclusion: Empowering Men’s Cardiovascular Health
While traditional CVD risk factors remain paramount, ignoring these lesser-known, male-disproportionate risks can lead to missed opportunities for prevention and early intervention. Men, in particular, should be encouraged to openly discuss symptoms like erectile dysfunction, fatigue, sleep disturbances, and mental health challenges with their healthcare providers. A proactive, holistic approach that considers these unique aspects of male physiology and lifestyle is essential for truly comprehensive cardiovascular care and empowering men to lead longer, healthier lives.