How does chronic stress impact the immune system?
The Intricate Link Between Mind and Body
Our immune system is a sophisticated network designed to defend the body against infections and diseases. While many factors influence its efficacy, one often underestimated culprit is chronic stress. In modern life, prolonged psychological or physical stressors are increasingly common, and their pervasive impact extends far beyond mental well-being, directly compromising our body’s defense mechanisms.
Understanding this connection is crucial for maintaining overall health. When stress becomes a constant companion, it triggers a cascade of physiological changes that can disarm our immune system, leaving us vulnerable. This article delves into the science behind how chronic stress impacts immunity, from hormonal shifts to cellular changes, and explores the resulting health implications.

The Body’s Stress Response Mechanism
When faced with a perceived threat, the body activates its ‘fight or flight’ response, a survival mechanism orchestrated primarily by the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system. This acute response is beneficial, preparing the body to react quickly to danger. However, chronic stress occurs when this response remains activated for extended periods, even in the absence of immediate physical threats.
Hormonal Cascade: Cortisol’s Role
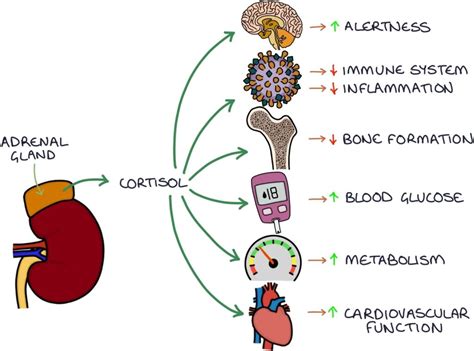
A key player in the stress response is cortisol, often referred to as the ‘stress hormone.’ In short bursts, cortisol can be anti-inflammatory and even enhance immune function, mobilizing immune cells to areas of the body that might need protection in an emergency. But under chronic stress, consistently elevated cortisol levels begin to have the opposite effect.
Prolonged exposure to high cortisol acts as an immunosuppressant. It inhibits the production of pro-inflammatory cytokines, reduces the number of lymphocytes (white blood cells crucial for fighting infection), and impairs the function of natural killer (NK) cells, which are vital for destroying virus-infected cells and tumor cells. Essentially, the immune system becomes less responsive and less capable of mounting an effective defense.
How Chronic Stress Weakens Immunity
Suppression of Immune Cells
Beyond cortisol, chronic stress directly affects the production and function of various immune cells. It can reduce the number of T-cells, which are critical for cell-mediated immunity, and B-cells, responsible for antibody production. This diminishes the body’s ability to recognize and destroy pathogens and to remember previous infections, making future encounters more dangerous.
Fueling Chronic Inflammation
Paradoxically, while acute stress initially suppresses inflammation, chronic stress can lead to chronic low-grade inflammation. This occurs because prolonged exposure to stress hormones can desensitize immune cells to cortisol’s regulatory effects. When these cells become less responsive to cortisol, they release inflammatory chemicals (cytokines) unchecked, leading to persistent, low-grade inflammation throughout the body. This chronic inflammation is a known risk factor for various diseases, including cardiovascular disease, diabetes, and certain cancers.

Real-World Health Implications
The cumulative effect of these changes is a compromised immune system, leading to several tangible health consequences:
- Increased Susceptibility to Infections: Individuals experiencing chronic stress are more prone to catching common colds, flu, and other viral or bacterial infections. Vaccinations may also be less effective.
- Slower Wound Healing: The inflammatory response crucial for wound repair is disrupted, leading to delayed healing of injuries and incisions.
- Exacerbation of Autoimmune Conditions: Chronic stress can trigger flare-ups or worsen symptoms in people with autoimmune diseases like rheumatoid arthritis, lupus, or psoriasis.
- Increased Risk of Chronic Diseases: The link between chronic inflammation and diseases like heart disease, type 2 diabetes, and certain cancers is well-documented.
Strategies to Mitigate Stress’s Impact
While eliminating stress entirely from life is unrealistic, managing its chronic effects is vital for immune health. Here are some effective strategies:
- Mindfulness and Meditation: Practices like mindfulness meditation can significantly reduce stress hormones and improve immune function.
- Regular Physical Activity: Exercise is a powerful stress reliever and can boost the immune system by increasing the circulation of immune cells.
- Adequate Sleep: Sleep deprivation increases stress hormones and impairs immune function. Aim for 7-9 hours of quality sleep per night.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients for immune support and helps regulate inflammation.
- Social Connection: Strong social ties can buffer the effects of stress and positively influence immune health.
- Professional Support: Consider therapy or counseling for persistent stress or anxiety.

Conclusion
The immune system is not an isolated entity; it is deeply intertwined with our mental and emotional state. Chronic stress acts as a silent saboteur, gradually eroding our body’s natural defenses and leaving us vulnerable to a host of health problems. Recognizing the profound impact of prolonged stress on immunity underscores the importance of proactive stress management. By adopting healthy lifestyle practices and seeking support when needed, we can bolster our immune system, maintain resilience, and safeguard our long-term health against the invisible threats of chronic stress.