How do certain environmental toxins disproportionately affect male reproductive health and fertility?
The Invisible Threat: Environmental Toxins and Male Fertility
Male reproductive health and fertility are facing an unprecedented challenge, with declining sperm counts and increasing rates of reproductive disorders reported globally. While genetics and lifestyle factors play a role, growing evidence points to environmental toxins as a significant, and often disproportionate, contributor to this crisis. Our modern world exposes us daily to a cocktail of chemicals that can profoundly disrupt the delicate processes essential for male reproduction.
Understanding the Primary Toxic Culprits
A range of environmental contaminants has been identified as threats to male fertility. These include:
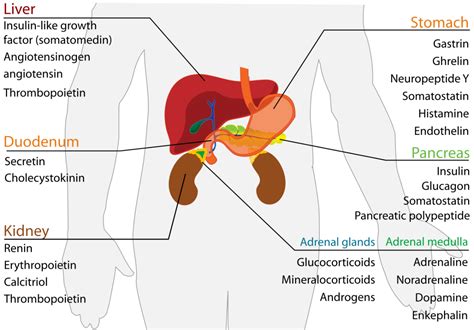
- Endocrine-Disrupting Chemicals (EDCs): Perhaps the most insidious, EDCs are synthetic chemicals that interfere with the body’s endocrine (hormone) system. Common EDCs include phthalates (found in plastics, personal care products), Bisphenol A (BPA, in food packaging, plastics), polychlorinated biphenyls (PCBs), dioxins, and certain pesticides. They can mimic, block, or alter natural hormones, especially androgens (male hormones) and estrogens.
- Pesticides and Herbicides: Agricultural chemicals like organochlorines, organophosphates, and glyphosate can directly toxic to reproductive cells and interfere with hormone synthesis and action.
- Heavy Metals: Lead, cadmium, mercury, and arsenic, found in contaminated water, food, and industrial emissions, are known neurotoxins and can also directly damage testicular tissue and sperm.
- Air Pollution: Particulate matter and polycyclic aromatic hydrocarbons (PAHs) from vehicle emissions and industrial processes can induce oxidative stress and inflammation, impacting sperm quality.
Mechanisms of Disruption: How Toxins Target Male Reproduction
Environmental toxins compromise male reproductive health through several pathways:
- Hormone Imbalance: EDCs are notorious for disrupting the hypothalamic-pituitary-gonadal (HPG) axis, the central regulator of male hormone production. They can decrease testosterone synthesis, alter its metabolism, or block its receptors, leading to reduced sperm production (spermatogenesis) and quality. Some EDCs also exhibit estrogenic activity, shifting the delicate androgen-estrogen balance crucial for male reproductive function.
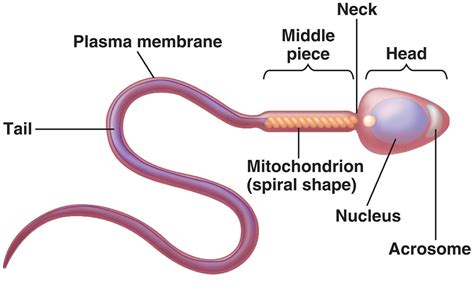
- Sperm Quality Degradation: Toxins can directly impair sperm development and maturation, resulting in lower sperm count (oligospermia), reduced motility (asthenozoospermia), abnormal morphology (teratozoospermia), and decreased viability.
- DNA Damage: Many environmental pollutants induce oxidative stress, leading to DNA fragmentation within sperm. Damaged sperm DNA can affect fertilization rates, embryo development, and potentially lead to genetic abnormalities in offspring.
- Testicular Dysfunction: The testes are highly vulnerable. Toxins can damage Leydig cells (which produce testosterone) and Sertoli cells (which support sperm development), impairing their vital functions. Exposure during critical developmental windows, such as in utero or during puberty, can lead to conditions like cryptorchidism (undescended testes) and hypospadias.
The Disproportionate Impact on Males
While environmental toxins affect both sexes, there are several reasons why males may experience a disproportionately severe impact on their reproductive health:
- Complexity of Spermatogenesis: The process of producing millions of sperm daily is incredibly intricate and hormonally regulated, making it highly susceptible to subtle disruptions. This continuous cell division also presents more opportunities for DNA damage.
- Androgen Sensitivity: Male reproductive development and function are exquisitely dependent on precise androgen signaling. EDCs that interfere with testosterone production or action can have profound and immediate effects.
- Testicular Vulnerability: The testes are a primary target organ for many heavy metals and EDCs. Their unique cellular composition and high metabolic activity can make them particularly vulnerable to toxic insults.
- Exposure Routes and Accumulation: Specific occupational exposures or lifestyle patterns might lead to higher levels of certain toxins in males. Moreover, some toxins accumulate in fat tissue, leading to prolonged exposure.
Long-Term Consequences and Prevention
The implications of toxic exposure extend beyond immediate fertility issues, potentially contributing to higher rates of testicular cancer and other male reproductive disorders. Furthermore, damaged sperm DNA could have intergenerational effects.
Mitigating this threat requires a multi-faceted approach:
- Policy and Regulation: Stricter regulations on the production and use of known EDCs and heavy metals are crucial.
- Consumer Awareness: Educating the public on how to identify and avoid products containing harmful chemicals (e.g., choosing BPA-free products, reducing plastic use, opting for organic foods).
- Lifestyle Modifications: Reducing exposure to pesticides by washing produce thoroughly, filtering tap water, and minimizing exposure to industrial pollutants.
Conclusion
The evidence is clear: environmental toxins are a significant and disproportionate threat to male reproductive health and fertility. By understanding the sources of these chemicals and their mechanisms of action, and by advocating for stricter controls and making informed lifestyle choices, we can collectively work towards safeguarding male reproductive health for current and future generations. Addressing this invisible crisis is not just a health issue, but a societal imperative.