How might changing sleep patterns impact a man’s testosterone levels as he ages?

The Crucial Link Between Sleep and Male Hormonal Health
Testosterone is a cornerstone of male health, playing vital roles in energy levels, muscle mass, bone density, libido, and mood. While its decline with age is a natural process, often referred to as andropause, the extent and timing of this decline can be significantly influenced by various lifestyle factors – chief among them, sleep. As men get older, their sleep patterns undergo noticeable changes, raising critical questions about how these shifts might impact their testosterone levels and overall well-being.
The Intricate Dance: Testosterone Production and Sleep Stages
Testosterone is not produced at a constant rate throughout the day; its synthesis is highly synchronized with our circadian rhythm and sleep cycle. Studies have shown that the majority of a man’s daily testosterone production occurs during sleep, particularly during deep REM (Rapid Eye Movement) and slow-wave sleep. Disruptions to these crucial sleep stages can directly impede the body’s ability to produce this vital hormone effectively.
Typically, testosterone levels peak in the early morning, coinciding with the end of a full night’s rest. This pulsatile release mechanism relies on uninterrupted, quality sleep. When sleep is fragmented or insufficient, this natural rhythm is thrown off, leading to a diminished nightly surge of testosterone.

Age-Related Shifts in Sleep Architecture
As men age, several common changes occur in their sleep patterns:
- Reduced Deep Sleep (Slow-Wave Sleep): This is the most restorative sleep stage, critical for physical recovery and hormone production. With age, the amount of time spent in deep sleep decreases significantly.
- Increased Sleep Fragmentation: Older men often experience more awakenings during the night, leading to less consolidated sleep.
- Earlier Bedtimes and Wake Times: A shift in circadian rhythm can cause older individuals to feel tired earlier in the evening and wake up earlier in the morning.
- Increased Prevalence of Sleep Disorders: Conditions like sleep apnea and restless legs syndrome become more common with age, further disrupting sleep quality.
These architectural changes directly impact the window of opportunity for optimal testosterone synthesis, often leading to lower circulating levels of the hormone.
The Direct Impact of Poor Sleep on Testosterone Levels
The evidence is compelling. Even a single week of insufficient sleep (e.g., 5 hours per night) has been shown to significantly reduce testosterone levels in young, healthy men, with drops ranging from 10% to 15%. For aging men, who may already be experiencing a natural decline, the impact can be even more pronounced.
Chronic sleep deprivation and poor sleep quality contribute to higher levels of cortisol, the stress hormone. Elevated cortisol can directly suppress testosterone production. Furthermore, disrupted sleep can impair the signaling pathways from the brain to the testes, reducing the release of luteinizing hormone (LH), which stimulates testosterone synthesis.
Symptoms of low testosterone, such as fatigue, decreased libido, erectile dysfunction, reduced muscle mass, and mood disturbances, can be exacerbated by or even directly caused by chronic poor sleep. This creates a vicious cycle: low testosterone can negatively affect sleep quality, which in turn further lowers testosterone.

Strategies to Optimize Sleep and Support Testosterone as You Age
While some age-related sleep changes are inevitable, many aspects of sleep quality can be improved through lifestyle adjustments:
- Prioritize Sleep Hygiene: Maintain a consistent sleep schedule, even on weekends. Create a dark, quiet, and cool bedroom environment.
- Limit Screen Time Before Bed: The blue light emitted from electronic devices can interfere with melatonin production, a hormone essential for sleep.
- Avoid Caffeine and Alcohol: Especially in the hours leading up to bedtime, as both can disrupt sleep architecture.
- Regular Exercise: Moderate physical activity during the day can improve sleep quality, but avoid intense workouts close to bedtime.
- Stress Management: Practices like meditation, deep breathing, or yoga can help calm the mind and facilitate sleep.
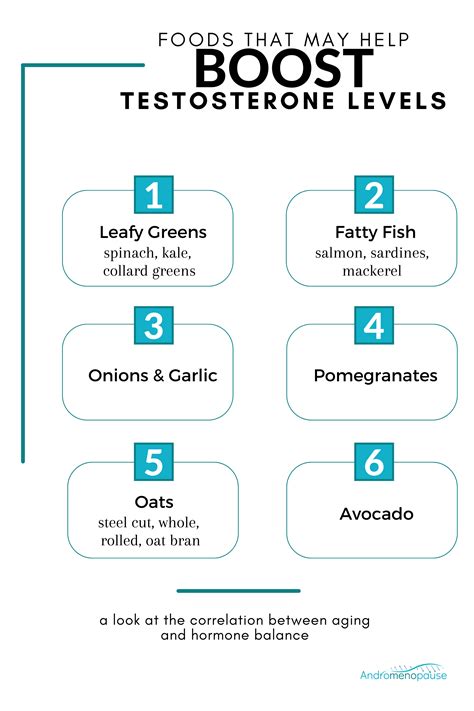
- Healthy Diet: A balanced diet rich in whole foods supports overall health, including hormonal balance and sleep.

When to Seek Professional Advice
If you are an aging man experiencing persistent fatigue, significant drops in libido, erectile dysfunction, unexplained weight gain, or mood changes, and you also struggle with sleep, it’s crucial to consult a healthcare professional. A doctor can assess your testosterone levels, investigate potential sleep disorders (like sleep apnea through a sleep study), and recommend appropriate interventions, which may include lifestyle modifications, hormone replacement therapy, or treatments for underlying sleep conditions.

Conclusion: Sleep as a Pillar of Aging Male Health
The relationship between changing sleep patterns and testosterone levels as men age is undeniable and profound. Prioritizing quality sleep is not just about feeling rested; it’s a fundamental strategy for maintaining hormonal balance, preserving vitality, and enhancing overall quality of life in the aging process. By understanding these intricate connections and adopting proactive measures, men can mitigate the impact of age-related sleep changes on their testosterone and strive for healthier, more energetic later years.